3D-Printed Thoracic Models in Realistic 3D for Surgical Training
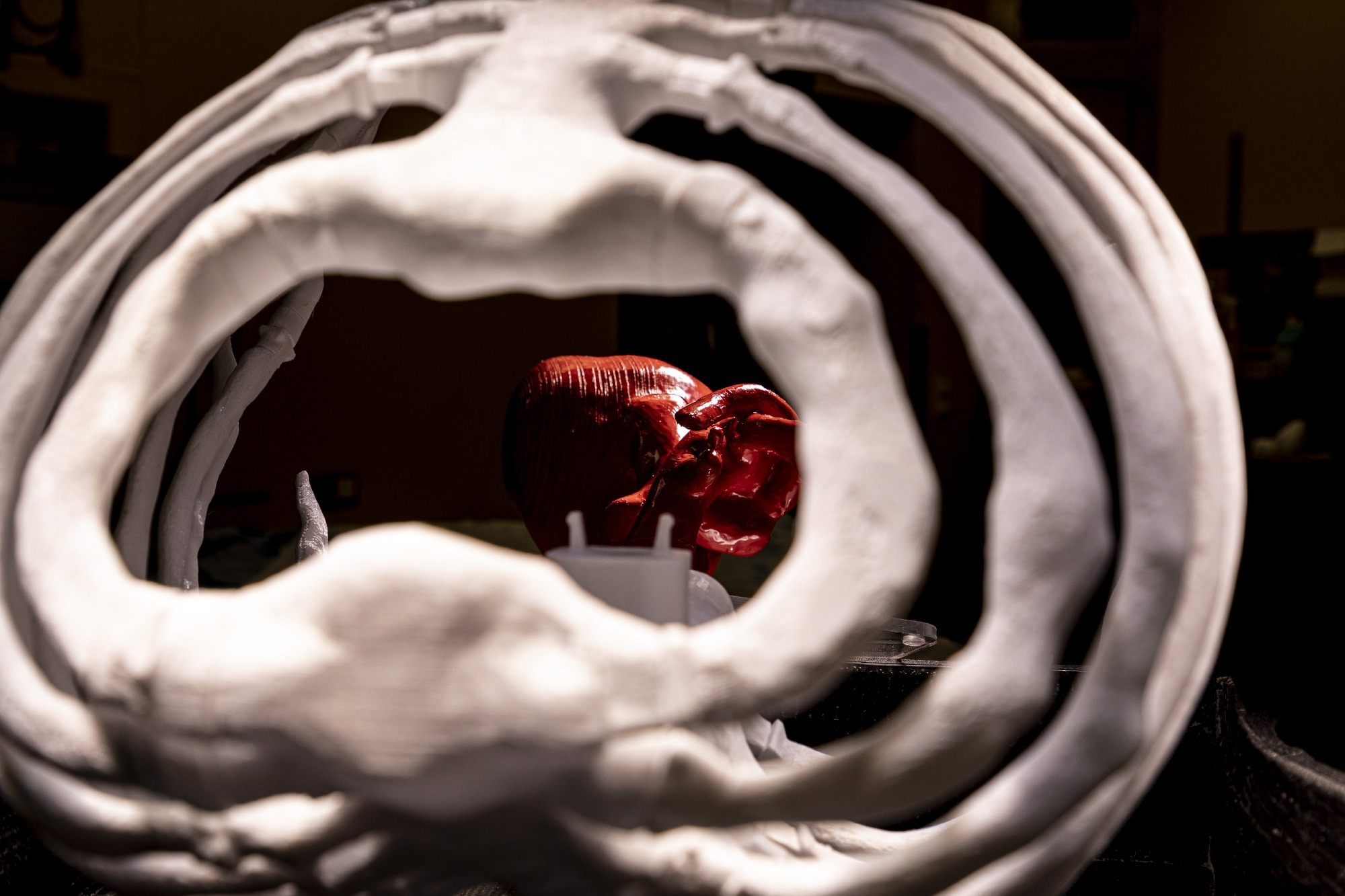
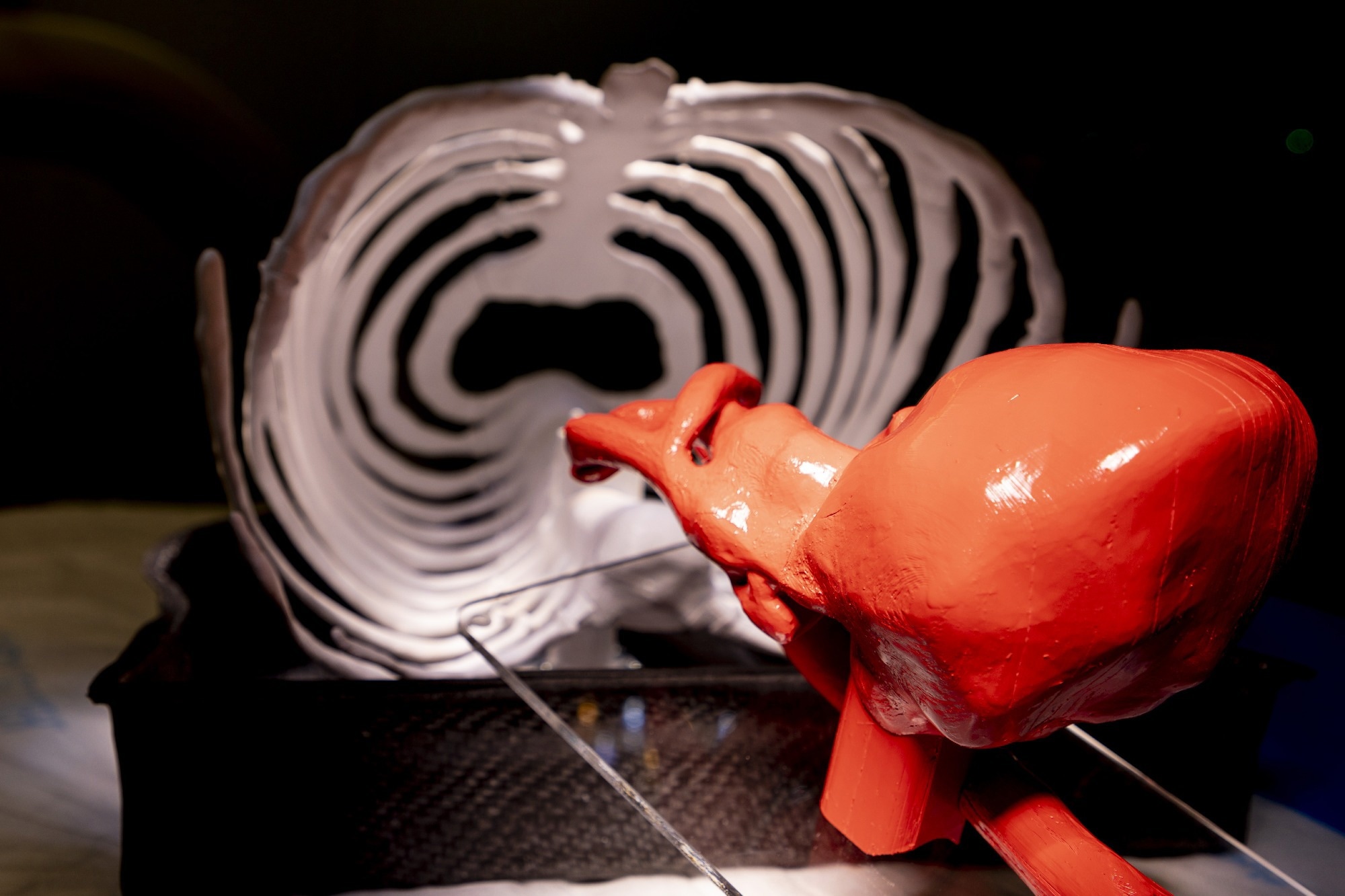
At MEDICA 2022, NewsMedical spoke with Heike and Thorsten Walles, co-founders of MD2B LifeScience, which provides realistic thorax models for surgical and implant training. These 3D-printed models could revolutionize how training is approached, with replaceable ribs that replicate the behavior of actual human bones.
Could you please introduce yourself and your professional background?
Heike Walles (HW): Heike Walles is the name of my daughter. I’m a biologist and I’ve worked for 25 years in the field of tissue engineering. I have extensive experience in the combination of cells and materials to create tissue-specific models.
Thorsten Walles (TW): My name’s Thorsten Walles. I am a surgeon who specializes in thoracic surgical, and I am the professor for thoracic surgeries at the University of Magdeburg. I also train young doctors. I also participate in the training programs of our National Society for Thoracic Surgery.
MD2B LifeScience is an outgrowth of Magdeburg University. It is 3D-printed Thorax models for medical training, and surgical planning. Why did you decide to develop a thoracic modeling method?
TW: It all started with one robotic surgery. When we use robotics the surgical procedures are very standardized, but I wanted to do a non-standardized approach for a rare tumor and had the problem of how I could rearrange the robotic setting for my patient. I wished there was a training device that would allow me to play with the planning of the surgery. I performed the surgery on my own, and it went smoothly. But that was the beginning of the idea.

Image credit: MD2B LifeScience
I asked the Engineering Department at our University whether it would be possible to generate some 3D thorax models, and the engineers told me that they could do it.
How was the development of your thorax models? And how has it changed from your original ideas?
TW: The engineers were faced with technical challenges and they solved them. We then decided to continue the idea and create a model to train young doctors and professionals for complex surgeries.
Our idea was presented to a national medical congress in September 2021. Other doctors also had ideas. Then, some industrial representatives remarked, ‘well you have the chest and you have the bones of the chest; this is useful for our implants’. They realized they could use these models to teach how to modify implants and apply implants. So the idea continued to grow.
Magdeburg University Hospital Image Credit
HW: Currently, for much surgical training, animals are used. If you’re a specialist in tissue engineering, you can create alternatives to animals models that perform the same functions. This is what our new technology allows us to achieve. Our new development allows us to create a realistic replica of the human spine for surgeons to train with. Second, bioartificial human tissue can be inserted, such as lung cancers.
Industry and academia are working together to develop electrodes and other devices that can be used for image-guided interventions. Many of these devices have to be used in conjunction with MRTs. So, we made modifications to our materials so you can use them under MRT.
We are constantly developing our product, and our company. This is thanks to the contributions of our shareholders as well as our scientific partners. Our development at MEDICA has already been embraced by many representatives from industry and academia.
What materials were used to create the models of the thorax?
HW: The material is what we are really trying to focus on so that model ribs can mimic human ribs physiologically. Because they behave exactly like human bones, it is how the industry can optimize its implants. It is cheaper to use a standard model for training, but it is possible to make a customized thoracic model from CT data if you are interested in creating one for your patient.

Magdeburg University Hospital Image Credit
The materials have been granted patents. The modified polymers used in the creation of bony structures. The collagen compounds are used to create bioartificial tissues.
What is the reason for improved models of the thorax?
TW: In minimally invasive thoracic surgery operations, the patient is lying on their side. The patient is lying on their side. A cavity is formed between the collapsed and chest wall. The surgeon uses his instruments to enter this area and performs the necessary operations. Sometimes he must flip the lung to reach the posterior or back side.

Magdeburg University Hospital Image Credit
It is difficult to perform these operative maneuvers within the narrow space of the thoracic cavity. There are many training models that allow you to practice minimally invasive operations in your abdomen and pelvis.
HW: So that you don’t see into our training models, we cover them with a soft tissue layer. Trainee doctors need to be able to reach the rib cage and feel the ribs. Our training model can include animal organs to simulate real operating conditions. You can perfuse and ventilate the organs.
What’s the advantage of 3D printing ribs?
HW: The additive production method allows for anatomically accurate imitation of the anatomical structure and ribs through mapping the cortical parts as well as the marrow cavity. A rib is not an harmoniously curved bone that has an oval cross-section. It can change its shape many times during the anatomical course.
Our models have been tested by a number of healthcare providers who supply implants for rib-re-fixation and are now being used for training medical professionals and doctors on how to use their implants.
After training in surgical or implant surgery, a broken rib can be exchanged easily. If necessary, it can also be broken again in another location.
These models can help reduce the use of animals for surgical training.
TW: Anatomically accurate representations of the human thoracic spine provide a more realistic environment for training than other animal models. Fresh or commercially available animal organs can be used for a realistic depiction of the visceral surgical steps, but in any case, this model reduces the need for laboratory animals. Our training models do not require special facilities. You can use them from any office or station in your seminar.
Magdeburg University Hospital Image Credit
Because every young doctor needs to know how to insert a tube into the chest, we started using our model for student training. Our model is far more manageable than the animal carcass that must be taken to the slaughterhouse.
Why is it so important that your models appear in MRIs or CTs?
TW: Although this feature is not required for surgeons, we thought that it could be useful for training interventional radiologists. You can also be trained in minimally invasive procedures on the chest such as radiofrequency ablations or percutaneous nodule biopsy.
How important is MEDICA a trade show to promote innovations like yours?
HW: As a young spinoff, this was extremely important. We wanted to determine if our development appeals in the right way to users, so it was very important to have ventures of this nature.

Image credit: MD2B LifeScience
TW: We are just at the beginning stages of development, so we have many options. As a small start up, we must decide what is more important and what the next steps are. MEDICA receives feedback from academics, professionals, and potential customers. MEDICA assists us in gaining a clear understanding of the market.
HW: It is amazing to realize that your ideas are relevant.
Is there any specific next step you’ll take to improve on your existing models?
HW: We will focus on finalizing the soft tissue coverage. Next, we’ll need to create models for the visceral organs of the thorax.
TW: Are the chest and rib cage the most interesting parts of the body? Is it necessary to work harder to create an idea for inner organs such as the heart or lungs? Do we need to use organs taken from animals? Or do we need artificial organs made of silicon, plastics, or something else? Although there are products on the market, we want to show the haptics and functions of organs so that the user can have a real experience during training and interventions. The question is, how close can we get to the artificial technologies we currently have?
About Heike Walles & Thorsten Walles
 Heike Walles, Dr. Born 1962 in Germany. 1982 – 1988 Studied Biology at the Justus-Liebig-University Gießen,Germany. 1989 – 1994 PhD thesis at the Ludwig-Maximilians University in Munich1999 – 2003 Post-Doc and Junior-Professor at Leibniz-Research-Laboratories for Biotechnology and Artificial Organs (LEBAO), Hannover Medical School, Hannover. 2004 – 2012 Head of Department Cellsystems, Fraunhofer-Institute Interfacial Engineering and Biotechnology (IGB), Stuttgart. 2009 – 2018 Full-Professor for Tissue Engineering and Regenerative Medicine, Julius-Maximilians-University, Würzburg. 2014-2018 Head of Fraunhofer Translational Center for Regenerative Therapies in Oncology and Musculoskeletal Diseases, Würzburg. Since 2018 Head of Core-Facility Tissue-Engineering, Otto-von-Guericke-University, Magdeburg, Germany. 2011 Co-founder of TissUse GmbH, Berlin. 2022 Cofounder of MD2B LifeSciences GmbH, Magdeburg
Heike Walles, Dr. Born 1962 in Germany. 1982 – 1988 Studied Biology at the Justus-Liebig-University Gießen,Germany. 1989 – 1994 PhD thesis at the Ludwig-Maximilians University in Munich1999 – 2003 Post-Doc and Junior-Professor at Leibniz-Research-Laboratories for Biotechnology and Artificial Organs (LEBAO), Hannover Medical School, Hannover. 2004 – 2012 Head of Department Cellsystems, Fraunhofer-Institute Interfacial Engineering and Biotechnology (IGB), Stuttgart. 2009 – 2018 Full-Professor for Tissue Engineering and Regenerative Medicine, Julius-Maximilians-University, Würzburg. 2014-2018 Head of Fraunhofer Translational Center for Regenerative Therapies in Oncology and Musculoskeletal Diseases, Würzburg. Since 2018 Head of Core-Facility Tissue-Engineering, Otto-von-Guericke-University, Magdeburg, Germany. 2011 Co-founder of TissUse GmbH, Berlin. 2022 Cofounder of MD2B LifeSciences GmbH, Magdeburg
Thorsten Walles, MD FETCS. German born in 1972. 1993-192000 Studied medicine in the Hanover Medical School. 1997-1998 A research stay at Johns Hopkins University in Baltimore, USA. 2000-2009 General and cardiac surgery training. 2009 specialist in thoracic and general surgery. Professor for Thoracic Surgery since 2017 and chief of the University Hospital Magdeburg’s Thoracic Surgery Service. Oncological surgery, minimally invasive Thoracic Surgery, Robot-Assisted Surgery, Pediatric Thoracic Surgery, and Thoracic Traumatology are the main areas of focus. 2011 Co-founder of TissUse GmbH (Berlin). 2022 Cofounder of MD2B LifeSciences GmbH in Magdeburg